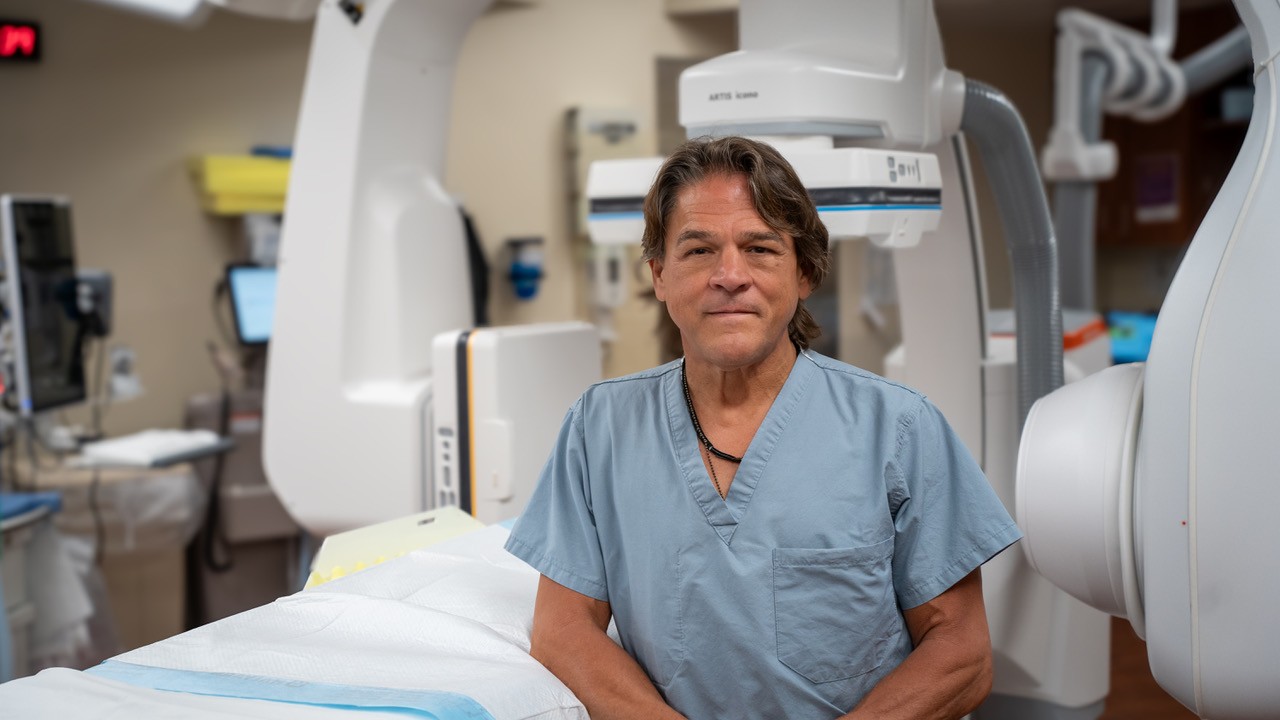
By: Steve Zanders, D.O., FCCP UPMC in Central Pa.
Every 40 seconds, someone in the U.S. has a stroke. Stroke is the fifth leading cause of death, the number one cause of disability, and can affect people of all ages — not just older adults. Rapid treatment for stroke is the key to preventing long-term disability.
A stroke occurs when blood flow and oxygen to the brain is interrupted (ischemic stroke) or when bleeding happens in the brain (hemorrhagic stroke). This loss of blood and oxygen causes two million brain cells to die every minute, so time is of the essence. The longer a stroke goes untreated, the higher the odds of permanent brain damage, disability, or death.
How the Stroke Affects the Brain
If you suspect someone may be suffering a stroke, think B.E. F.A.S.T:
· Behavior and Balance: Has the person had a change in behavior or lost their balance?
· Eyes: Ask the person if their vision has changed. Are their eyes moving abnormally or is gaze fixed?
· Face drooping: Ask the person to smile. Is one side of the face drooping?
· Arm weakness: Ask the person to raise both arms. Is one arm weak or numb?
· Speech trouble: Ask the person to repeat a simple sentence like “the sky is blue.” Is speech slurred or hard to understand?
· Time or Terrible headache: Is the person experiencing a terrible headache, especially the worst they’ve ever experienced? When it comes to stroke, time is crucial. If someone is experiencing any of these symptoms, call 9-1-1 immediately—even if the symptoms start to fade.
Depending on the severity of a stroke, someone may experience all these symptoms, or none at all.
Treatment and Life After Stroke
With all stroke treatments, time is critical. The procedures must be performed quickly after onset of symptoms. The goal is to restore blood flow to the brain as quickly as possible to prevent permanent brain damage or death.
There are specialized centers, including UPMC Harrisburg, that offer advanced therapies such as thrombectomy, or surgical removal of the blood clot, as well as neurosurgical and neurocritical care expertise for hemorrhagic strokes and all stroke complications. UPMC Harrisburg works closely with the other six UPMC hospitals in the region to coordinate safe and expedient care.
UPMC is cognizant and aware of the challenges patients face during and after a stroke. Treatment for post stroke complications often begins while patients are still in the hospital and can include medications, psychological therapies, visual, and optic rehabilitation, as well as addressing standard motor and sensory dysfunction.
Stroke patients begin rehabilitation within 12-24 hours, provided they are stable. Muscle weakness and depression, which often follow strokes, are addressed through treatment plans as soon as patients are
admitted. In cases where stroke has caused limited or extensive disability, inpatient rehabilitation begins within days of treatment, and upon discharge the patient may need ongoing physical therapy.
Physical changes that follow a stroke are the result of injury to the brain and may include one or more effects.
· Weakness or Paralysis
· Fatigue
· Communication challenges
· Memory deficits
· Emotional or behavioral changes
With fast and proper treatment, stroke patients can greatly improve health outcomes and recovery following a stroke. Stroke affects many functions of the body and it’s important that patients receive appropriate, quality rehabilitation with a specially trained team to overcome deficits and improve the chances for the best possible recovery.
Every patient’s recovery is different, but often stroke recovery takes three to 12 months and beyond. To maintain gains and work on evolving needs, patients must continue to work at their recovery. Learn more about UPMC Stroke Centers in Central Pa.
Dr. Steve Zanders is the associate medical director of critical care services and medical director of neurologic critical care, neuroendovascular and stroke care at UPMC in Central Pa.